![]()
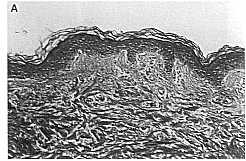
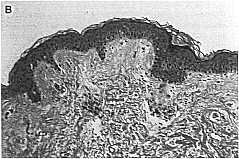
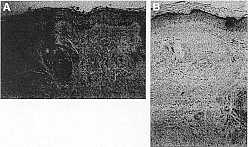
Preauricular skin A) pretreatment and B) 1 week after final treatment. Histologic appearance of forearm skin A) pre B) Post with slight thinning of the stratum corneum and slight dermal edema.
(Hematoxylin and eosin, original magnification 20x).
MEI-HENG TAN, MD,* JAMES M. SPENCER, MD, MS,* LUCIANE MONTEIRO PIRES, MD,* JYOTENDRA AJMERI, MBBC,* AND GREG SKOVER, PHDt
* Department of Dermatology, Mount Sinai School of Medicine, New York University, New York, New York, and tSkin Research Center, Johnson and Johnson Consumer Products, Skillman, New Jersey
BACKGROUND. Aluminum oxide crystal microdermabrasion has recently become popular for facial rejuvenation. Although it is a widely used technique with perceptible benefits, the clinical efficacy on photodamaged skin has yet to be established.
OBJECTIVE. To measure and quantify the effect of microdermabrasion on photodamaged skin.
METHODS. Ten subjects underwent one treatment a week for five to six treatments. Skin surface roughness, topography, elasticity, stiffness, compliance, temperature, sebum content, and histology were analyzed.
RESULTS. Subjectively, seven patients noticed a mild improvement. Physician analysis of clinical photography indicated mild improvement in the majority of patients. Objectively, immediately following treatment skin temperature increased, sebum con- tent decreased, and a temporary increase in skin roughness and mild flattening of some wrinkles occurred. Dynamic skin analysis demonstrated a perceptible decrease in skin stiffness and an increase in skin compliance. Histology showed slight orthokeratosis and flattening of rete ridges and a perivascular mononuclear cell infiltrate, edema, and vascular ectasia in the upper reticular dermis 1 week after completion of the series of treatments.
CONCLUSION. Immediately following the procedure, changes occurring in skin characteristics can be measured that are consistent with mild abrasion and increased blood flow. Objective biomechanical analysis demonstrated a statistically significant decrease in skin stiffness and an increase in skin compliance consistent with persistent edema. Subjectively, patients and physicians report a mild improvement in the majority of subjects. Histology showed dramatic vascular changes in the reticular dermis below the level of direct abrasion. The effect of negative pressure may result in these vascular changes.
ALUMINUM OXIDE CRYSTAL microdermabrasion, a technique developed in Italy in 1985, has recently become popular. It is a noninvasive, nonsurgical procedure used to revitalize and rejuvenate the skin. The device gently pulls the skin into a hand piece by mild suction which initiates the controlled flow of corundum particles. Dirt, oil, surface debris, and dead skin cells are removed by the impact of the particles on the skin’s surface. Because it’s a closed-loop process, debris and particles are collected in a reservoir and dis- carded after the procedure. The particle flow rate and vacuum pressure control the amount of particles impacting the skin. These factors, as well as movement of the hand piece over the surface and the number of passes, determine the degree of exfoliation. The treatment is typically performed in a series of 4-12 weekly visits taking 30-45 minutes. After the procedure there is a mild, transient erythema and a sensation described as a slight sunburn or windburn.
Articles have appeared in the lay and professional press regarding the procedure, however, there remains a void of objective clinical studies that demonstrate its effectiveness. Regardless of proven clinical efficacy, there has been an overwhelming perceived benefit in the skin’s appearance and texture from patients paying for a course of therapy.
What allows this device to be sold without appropriate clinical support is the decision by the u.s. Food and Drug Administration (FDA) that the device is not life sustaining and hence is classified as a type 1 de- vice. This classification does not require the manufacturer to establish performance standards for the instrument, only to agree to manufacture the device using good manufacturing practices (GMP) guidelines. Furthermore, in 1998 the FDA gave the instrument “exempt” status, eliminating the need for a clearance letter from the FDA in order to sell the device in the United States. Consequently, they have quickly be- come popular in the offices of plastic surgeons, dermatologists, and those who treat the skin, including spas, for the management of fine rhytides, photoaging, mild surgical and acne scars, active acne, dyschromias, and melasma. However, it will never be considered a treatment without rigorous clinical testing.
Only one study has been published examining the efficacy of this widely practiced technique. This study demonstrated the effectiveness of aluminum oxide crystal microdermabrasion in the treatment of facial scar- ring as determined by the treating physicians’ subjective appraisal of improvement.1 It was our intent to mea- sure the effectiveness of microdermabrasion on photo- damaged skin using a number of different methods capable of discriminating between superficial and substantial results.
Materials and Methods
Ten volunteer subjects with Fitzpatrick skin types I-III and photodamage (Glogau scale II and III) of the facial skin were recruited for the study. Pregnant candidates and those with a history of abnormal wound healing were excluded from the study. Women of childbearing potential provided documented evidence of reliable contraception. Informed consent was obtained from each patient. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in approval by the Mount Sinai School of Medicine Human Research Review Committee.
Subjects washed their faces before photography and mesurements were taken. Microdermabrasion was performed (Parisian Peel, Aesthetic Technologies Inc. Colorado Springs, CO) as per the manufacturer’s specifications; one treatment a week of the face at a vacuum pressure of 30 mmHg with the handpiece in contact with the skin for four passes over the face, and at a vacuum pressure of 15 mmHg with the handpiece in contact with the skin for two passes over periorbital skin, for a total of five to six treatments. Patients were advised to decrease sun exposure to the treated area during the study to minimize risk of postinflammatory hyperpigmentation. Measurements were performed before and after microdermabrasion on the first, second, and fifth visit. Final evaluations were performed 1 week after the final procedure.
Clinical Photography
Photographs were taken before and after the procedure with a Nikon N6006 camera, Nikon 60mm f/2.8 lens, and CSI Twin Flash (Canfield Scientific, Fairfield, NJ) using Kodak Kodachrome film. Replicate photographs were taken from 0 degrees, 45 degrees (right), and 45 degrees (left) using a standardized reproduction ratio of 1:6 (f/16) for full facial photographs and 1:3 (f/22) for close-up photographs. The subject was positioned in a head restraint, enabling comparative photographs to be taken throughout the study. Pre- and posttreatment photographs were assessed by two physicians and graded on a four-point scale: 0% change from baseline, no improvement; 1-250;0 change, mild improvement; 26-75% change, moderate improvement; 75-100% change, marked improvement.
Thermography
In order to document thermographic changes, one patient was positioned in front of the image receptor at a specified distance to capture thermographic changes before and after the procedure.
Sebum Content
Sebum content was measured with an automated sebumeter. The handpiece containing absorbent tape was calibrated in the device before use at each site. Seven sites were measured before and after the procedure, including right and left cheek, right and left forehead, right and left orbital, and chin. The handpiece is held in contact with the skin for 30 seconds and then repositioned in the device. Sebum content was measured in micrograms per square centimeter. Statistical analysis was performed on each site, at each visit, as well as a facial average using all sites.
Biomechanical Characterization
Skin elasticity, stiffness, and compliance were measured be- fore and after the procedure (BTC 2000, S.R.L.I. Inc., Nash- ville, TN). The BTC-2000 measures the response of the skin during dynamic stress created by suction. The instrument applies a linear negative pressure at a rate of 10 mmHg/sec over 1 cm of skin until 150 mmHg is achieved. An infrared targeting laser measures the vertical displacement of the skin during the cycle. Pressure and deformation are graphically displayed on the monitor and embedded biomechanical algorithms determine the aforementioned parameters based on the average of three repetitive cycles. Four sites on the face were analyzed and compared, including the right and left cheek and the right and left forehead.
Skin Surface Topography
Silicone skin replicas of the left orbital skin and left fore- head were made before and after the procedure to measure surface texture and topography using three-dimensional microtopography. The replicas were positioned underneath the light source, which is similar to a camera flash. The instrument projects sinusoidal intensity distributions of the replica and reconstructs the data using temporal phase-shift algorithms to generate three-dimensional images. Mathematical equations embedded in software analyze the different segments and re-create a three-dimensional surface profile. Algorithms contained in the evaluation software permit rough- ness to be calculated from the acquired surface profile.
Roughness (Ra) is the arithmetic average of the absolute values of all points of the profile. In other words, Ra is the height of the rectangle with the same length and surface as the profile enclosed in the specified sector.
Histology
Subjects were asked to provide a preauricular biopsy speci-men, however, refusal did not exclude them from the study. Preauricular 2 mm punch biopsy specimens of two patients were taken before and 1 week after final treatment and evaluated for cellular and dermal histologic changes. Assessment of the dermal architecture was performed using specific stains for collagen (trichrome) and elastin (elastin-van Gieson).
In addition, two healthy men with no history of abnormal wound healing underwent one treatment consisting of four passes of microdermabrasion at a pressure of 65 mmHg over a 2 cm X 2 cm area of normal skin. Patient A under- went treatment on skin of the volar forearm; patient B was tested on the dorsal forearm. Three millimeter punch biopsy specimens were obtained before and immediately after treatment for light microscopy to compare histologic changes after a single treatment. Photography of the treatment areas was performed before and after treatment.
Adverse Events
Assessments of efficacy and safety were performed at each treatment visit, when the investigator evaluated skin appearance and local adverse reactions based on physical examination of the treated area and the subject’s report.
Results
In the group with facial photo damage, nine patients completed at least five treatments and returned 1 week after the final treatment for evaluation. Physician evaluation of clinical improvement revealed five of the nine subjects as having mild (1-25%) and one of nine as moderate (26-75%) improvement on the four-point assessment scale (Figure 1). One patient dropped out for unrelated reasons after three treatments. Evaluation after only three treatments also showed mild improvement. In summary, 7 of the 10 subjects showed at least mild improvement in three to five treatments.
Subject Assessment
Seven of the 10 subjects who participated noticed a clinical improvement as a result of the microderm- abrasion treatments. Among these seven was the patient who had only three treatments. Of these, four had Fitzpatrick skin type i and three had Fitzpatrick skin type II. Of the three subjects who reported no improvement, one had Fitzpatrick skin type II and two had Fitzpatrick skin type III. Of the seven who noticed clinical improvement, five were Glogau group II and two were Glogau group III. All three patients who reported no improvement were Glogau group III.
Skin Thermography
Thermography was performed at the first visit before and after the procedure on one patient. Immediately following the procedure, thermal photography showed increased skin temperature, consistent with increased blood flow
Sebum Analysis
The sebumeter showed a dramatic decrease in surface sebum immediately after each procedure, but this effect did not persist between treatments. All subjects washed with soap less cleanser prior to measurement. Normal sebum levels for facial skin are in the range of 66-250 JJ.g/cm2. Therefore levels recorded indicate removal greater than cleansing alone
Biomechanical Characterization
Dynamic skin analysis demonstrated inconsistent changes in skin stiffness and compliance before and after the procedure irrespective of patient or measurement site. How- ever, analysis of cheek skin demonstrated a sequential decrease in skin stiffness and an increase in skin compliance throughout the study. Statistical analysis com- paring baseline and final measurements indicated that
these changes were statistically significant
Skin Surface Topography
Roughness analysis of impressions from the crowsfeet area revealed a temporary increase in skin roughness and a mild flattening of some wrinkles immediately after treatment (Figure 5). The increased roughness is consistent with a mild abrasion. One week after the first treatment this effect was gone. Similarly these changes were seen immediately after the final treatment, but did not significantly persist 1 week later in the majority of patients at the final evaluation thus indicating a transient effect consistent with mild abrasion
and edema that resolves in less than 1 week. However, two patients showed a significant decrease in rough- ness (or increased smoothness) at the final evaluation (patients 3 and 8). These two patients had the greatest increase in roughness immediately after the first treatment, suggesting these two had the greatest abrasion initiallv.
Histology
Preliminary histologic evaluation was performed on the forearm of two male volunteers. Four “passes” at a setting of 65 mmHg is considered an aggressive setting and produced a significant erythema of the skin. Light microscopy showed a slight thinning of the stratum corneum and slight dermal edema after treatment (Figure 8B). No change in the viable epidermis or dermis of treated skin was noted when compared to controls. Despite the minimal abrasion, the visible erythema persisted 5-6 days after treatment in both subjects.
Hitologic studies comparing preauricular skin in two subjects before and 1 week after final treatment showed a slight increase in orihokeratosis, a slightly diminished rete ridge pattern of the epidermis, and in the upper reticular dermis a perivascular mono- nuclear cell infiltrate, slight edema, and vascular ectasia in both posttreatment specimens. There was no significant change in collagen or elastin content.
Adverse Events
There were no serious adverse events. Two patients experienced mild adverse events. These included moderate skin dryness after the fourth treatment which re- solved 2 weeks after the last treatment and irritated, scaly, increasingly pink eyelids after the second treatment which resulted in stopping subsequent treatments four and five to the eyelids. The irritation resolved 1 week after stopping treatment to this area.
Conclusion
Microdermabrasion is a simple, rapid procedure that can be repeated easily at short intervals. It is painless, bloodless, noninvasive, and minimally inconvenient for the patient, with little or no disruption in quality of life.
Aluminum oxide crystals are an inert ceramic, chosen as an abrading substance for their hardness, which is second only to diamonds. This material has been utilized as a dental abrasive and in joint replacement procedures for many years. It is an inert compound, insoluble in water, and due to its weight it is thought to drop to the ground following the procedure rather than being aerosolized as a dust where it could present a respiratory hazard. Despite its benign nature and experience with this material several potential health hazards have been raised. These include ocular complications such as eye irritation, adherence of crystals to the cornea, and increased risk of flares in patients with a history of recurrent herpes simplex infection. Exposure to aluminum oxide dust has been associated with pulmonary lung fibrosis, and laryngeal and tracheal papillomas. Chronic aluminum (but not aluminum oxide) exposure has been associated with impaired cognitive performance and aluminum may be involved in the senile plaques of Alzheimer’s disease.
After one treatment of four passes at 65 mmHg (described as an extremely aggressive setting by the manufacturer) only a slight abrasion of the stratum corneum is produced. However, a significant visible erythema occurred lasting 5-6 days after the procedure, indicating a biologic response. It is unlikely that partial loss of stratum corneum accounts for the persistent erythema seen.
In Fitzpatrick skin type I-III subjects with Glogau class II-III photodamage, a series of five to six weekly treatments with four passes of aluminum oxide crystal microdermabrasion at 30 mmHg produced a mild noticeable improvement in the appearance of facial skin in the majority of patients as reported by both physician and self-evaluation. An increase in skin roughness, slight flattening of wrinkles, and a significant decrease in sebum content can occur after each treatment. However, these changes are transient and did not remain during the course of therapy or the duration of the study. It is interesting to note that the two patients that showed the greatest increase in skin roughness after the first treatment showed a marked decrease in skin roughness at the 6-week time point. This may suggest that robust initial exfoliation may initiate a chain of events that leads to noticeable skin smoothness over the course of therapy.
Repetitive abrasion of the skin with a cream preparation containing aluminum oxide granules has been shown to cause an increase in desquamation rate, cutaneous blood flow, epidermal thickness, and skin extensibility. However, no significant inflammation or change in degree of elastosis were detected histologically. Slight fibrotic changes including granulomas in the upper dermis, normalization of the stratum corneum, epider- mal thickening, and increased collagen deposition in the papillary dermislo after a series of microdermabrasion treatments have been reported. It is postulated that new collagen and glycosarninoglycan deposition can occur.lO,ll However, we did not detect these changes histologically.
After a series of treatments our histology showed some epidermal changes consistent with abrasion, but more dramatic changes were present in the reticular dermis and are vascular; vascular ectasia, perivascular mononuclear cell infiltrate, and dermal edema are all seen 1 week after the final treatment. This may pro- duce the color change and improved appearance noted by patients and physicians. The biomechanical assessment with the dynamic skin analyzer recorded changes consistent with these histologic observations. A signifi- cant decrease in skin stiffness was noted on the cheeks but not on the forehead during the course of treatment. This change persisted for 1 week after the last treatment. A parallel increase in skin compliance was also seen during the course of the study. These changes are consistent with increased edema and hydration of the skin, similar to a stiff, dry sponge becoming a soft, pliable sponge as it becomes hydrated. The depth of these changes is well below the level of direct abrasion. It is very likely that this technique may involve a mechanism other than abrasion. The aspiration system used to suck away the used aluminum oxide crystals may help promote tissue blood supply. It may be possible that the effect of negative pressure results in the vascu- lar changes observed in our study and is responsible for the improved appearance noted by physicians and patients.
Acknowledgments This study was funded by a grant from Aesthetic Technologies Inc. The authors would like to ex- press our sincere appreciation to Glicia Spencer and Diana Martinez for their participation in data collection, and Dr. Greg Payonk, Johnson & Johnson CPWWRD&E, for creation and development of image acquisition methods, soft- ware, and analysis of skin surface topography.
References
1. Tsai RY, Wang CN, Chan HL. Aluminum oxide crystal micro- dermabrasion: a new technique for treating facial scarring. Dermatol Surg 1995;21 :539-42.
2. Warmuth IP, Echt A, Scarborough DA. Microdermabrasion-a new rejuvenation treatment option. Cosmet DermatoI1999;12(10):7-10.
