![]()
JENIFER R. LLOYD, DO
Northeastern Ohio Universities College of Medicine, Youngstown, Ohio

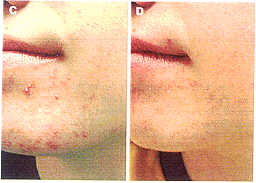
Figure 1. A-F) Pre- and posttreatment photographs demonstrating clinical improvement of acne following eight microdermabrasion treatments. Dermato/ Surg 27:4:Apri/2001
BACKGROUND. Microdermabrasion is a superficial peeling modality that has become quite popular with our patients and the media.
OBJECTIVE. To evaluate the use of microdermabrasion in patients with acne.
METHODS. Twenty-five patients with grade II-III acne were en- rolled into this pilot study. All patients were under dermatologic care and were maintained on their acne medications throughout the study. Patients received eight microdermabrasion treatments at weekly intervals. The results were documented with before and after photographs and evaluated for clinical improvement.
RESULTS. Twenty-four patients completed the study with 38% (9/24) having excellent results, 34% (8/24) with good results, 17% (4/24) with fair results, and 12% (3/24) with poor results. Ninety-six percent (23/24) of patients were pleased with their peel results and would recommend this procedure to others.
CONCLUSION. The use of microdermabrasion in this pilot study appeared to produce a positive effect on the improvement of acne.
OVER THE PAST few years, use of the microdermabrasion procedure has experienced widespread growth among physicians as well as aestheticians for a host of conditions, despite few studies concerning its safety and efficacy.1.2 The majority of information concerning microdermabrasion is provided by the vendors and is echoed in the popular press.
Microdermabrasion is a process that uses aluminum oxide crystals and negative pressure to superficially peel the surface of the skin. It has been well documented that superficial peeling agents are beneficial in the treatment of acne.3-7 This pilot study was done to assess the use of the microdermabrasion process to aid in the treatment and resolution of acne.
Materials and Methods
Twenty-five patients (6 males and 19 females) with grade II- III acne were entered into the institutional review board- approved study.
These patients ranged in age from 11 to 20 years of age (average age 15.5 years). All patients were under dermatologic care for their acne at the time of their enrollment and remained on their acne medications while receiving the microdermabrasion treatments. All patients were on an oral antibiotic as well as topical therapy, including a topical retinoid for 96% (24/25) of the patients. Medications were adjusted if necessary during the course of treatment. Patients were excluded from the study if they had been on isotretinoin or were currently pregnant. Pretreatment photographs were obtained using Mirror Image (Can- field Computer Systems, Fairfield, NJ). Eight microderm- abrasion treatments were performed on the full face using the Parisian Peel medical microdermabrasion device (model DMX, Aesthetics Technologies, Inc., Broomfield, CO). These treatments were spaced at 7- to 10-day intervals. The treatment power started at an average of 26.67 cmHg and was increased, as tolerated, with each treatment. The final power averaged 41.11 cmHg. Posttreatment photographs were obtained 2 weeks after the last treatment. The results were assessed by the physician as well as two nurses by comparing pre- and posttreatment photographs for overall improvement of acne lesions and postinflammatory changes. The following graded scale was used: excellent (76-100%), good (51-75%), fair (26-50%), and poor (0-25%). Patients were also surveyed to assess their perception of the treatment process and results.
Results
Twenty-four patients completed the study according to protocol. One patient was withdrawn from the study after completing only four peels to begin isotretinoin therapy. Assessment of the patients' treatment results were photographically evaluated (Figure 1). Figure 2 shows the breakdown of the patients' results. Overall 38% (9/24) of patients achieved excellent results, 34% (8/24) of patients had good results, 17% (4/24) had fair results, and only 12% (3/24) had poor results.
All patients tolerated the procedure well. Erythema was noted immediately following the procedure which resolved within 24 hours. No other adverse effects were noted during the study.
All 24 patients responded to the follow up survey. The patient survey results revealed 92 % (22/24) of the patients noticed an improvement in their skin with the microdermabrasion process. Ninety-six percent (23/ 24) of the patients were pleased with their peel results and would recommend this procedure to others.
Discussion
Since the publication of the first article on microderm- abrasion in 1995,1 this technique has been driven by the media and consumer market.
The paucity of literature on this topic led us to undertake this pilot study to evaluate the use of microdermabrasion in acne.
Acne is a common problem that begins in puberty and can continue into adulthood. Numerous oral and topical products are available for the treatment of this condition.
Several studies have been done showing the efficacy of glycolic acid4,s and salicylic acid6,7 peels in the resolution of acne and acne scarring. The results of this study suggest that microdermabrasion is another modality useful for the improvement of acne.
The Parisian Peel process directs a stream of aluminum hydroxide (AyO3) microcrystals onto the skin surface and then removes the particles with vacuum suction. The operator moves the handpiece evenly over the skin using three passes: one vertical, one horizontal, and one oblique, to prevent streaking. Any problem areas, such as comedones receive additional passes using the foot pedal for a higher compression rate.
Seventy-one percent of the patients with grade II-III acne who entered into this study received a greater than 50% improvement in their acne. The most prominent improvement was noted with postinflammatory acne changes and the overall skin qualitv. One patient with grade III acne worsened during the peel process and was removed from the study to begin isotretinoin therapy.
During this study, patients remained on their oral and topical therapy. Being a pilot study without a control group, it could be argued that the patients' acne improved with the prescription products alone. Further studies using a control group would be beneficial to show the true efficacy of the microdermabrasion process In acne.
The advantage offered by microdermabrasion over other peeling modalities is the ability to provide a nonsurgical, nonchemical, noninvasive procedure that can be done safely by trained office personnel. This procedure is well tolerated and has a very high patient satisfaction level.
The use of microdermabrasion in this pilot study appeared to produce a positive effect on the improvement of acne. These promising findings warrant further investigation.
References
1. Tsai RY. Wang CN, Chan HL. Aluminum oxide crystal microdermabrasion. A new technique for treating facial scarring. Dermatol Surg 1995j21:539-42.
2. Newman I, Hopping S, Patterons R, Saxton S. Power peeling (micro skin abrasion). Intl Cosmet Surg 1998-1999;6:101-5.
3. Moy LS, Murad H, Moy RL. Superficial chemical peels. In: Wheeland RG, eds. Cutaneous Surgery. Philadelphia: WB Saunders, 1994:463-78.
4. Wang CM, Huang CL, Hu CT. Chan HL. The effect of glycolic acid on the treatmenr of acne in Asian skin. Dermatol Surg 1997;23:23-9.
5. Atzore L, Brundu MA, Orru A, Biggio P. Glycolic acid peeling in the treatment of acne. J Eur Acad Dermatol VenereoI1999;12:119-22.
6. Kligman DJ Kligman AM. Salicylic acid as a peeling agent for the treatment of acne. Cosmet DermatoI1997;10:44-7.
7. Grimes PE. The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups. Dermatol Surg 1999;25:18-22.
@ 2001 by the American Society for Dermatologic Surgery, Inc. . Published by Blacklvell Science, Inc ISSN: 1076-0512/01/$15.00/0 . Dermatol Surg 2001;27:329-331
J. R. Lloyd, DO has indicated no significant interest with commercial supporters.
Address correspondence and reprint request~ to: ]enifer Lloyd, DO, Lloyd Dermatology and Laser Center, 8060 Market St., Youngstown, OH 44512, or e-mail: jrI2@neoucom.edu
